Managing Adult Malnutrition
Managing Adult Malnutrition
A COMMUNITY HEALTHCARE PROFESSIONAL GUIDE TO THE
NUTRITIONAL MANAGEMENT OF PATIENTS DURING AND AFTER COVID-19 ILLNESS
Overview
The contents of this page can also be DOWNLOADED IN PDF FORMAT
This resource has been endorsed by the British Dietetic Association (BDA), the Royal College of Nursing (RCN) and the British Association of Parenteral and Enteral Nutrition (BAPEN).
The severe symptoms and consequences of COVID-19 may exacerbate malnutrition already present but may also predispose a previously well-nourished patient to the risk of malnutrition as a result of elevated nutritional requirements associated with infection arising at a time when appetite is diminished1. This highlights the importance of nutritional screening and the provision of good nutritional care during this pandemic.
Whilst 32% of COVID-19 cases will require hospitalisation, 68% of those affected will remain in the community2. Within the community, disease related malnutrition is prevalent amongst those of older age and those with chronic diseases3, underlying malnutrition in these patients may impair the immune response4 and further worsen COVID-19 severity. In addition individuals who have been discharged from hospital may need ongoing nutritional rehabilitation.
The Malnutrition Pathway has collated expert consensus, best practice and available evidence to support community healthcare professionals during COVID-19. The information on these pages has been designed to assist healthcare professionals in identifying nutritional issues, including the likelihood of malnutrition, when undertaking virtual consultations, in patients who are under their care. The resources - a pathway of care to support healthcare professionals and corresponding patient leaflets- are intended to help provide timely and appropriate nutritional advice. It includes dietary advice and use of oral nutritional supplements (ONS) where required, to support patients during and after an infection of COVID-19, who are being cared for at home or who have been recently discharged from hospital.
The information in this section is derived from the Managing Malnutrition in COPD and Managing Malnutrition in the Community patient materials, taking into account what we know about the nutritional management of patients with COVID-19 at the time of development (May 2020). It is aimed at adults and does not include advice on enteral tube feeding. It should not replace individual advice from a qualified dietitian (check patient's medical record).
(Further advice on enteral tube feeding can be found HERE)
Respiratory Issues
Respiratory issues observed in severe cases of COVID-19 have a similar presentation to infective exacerbations of respiratory diseases such as chronic obstructive pulmonary disease (COPD). Symptoms that can affect dietary intake include:
- Coughing and breathlessness
- Gas trapping and early satiety, caused by gulping air whilst eating5
- Dry mouth due to breathing through the mouth, use of inhalers and oxygen therapy5
Changes to Taste and Smell
Loss of taste and smell have been reported in patients with COVID-196,7 and may further impact appetite and desire to eat.
Temperature and Infection
The infection triggers an inflammatory response and a rise in body temperature7 which can suppress appetite and alter metabolism, increasing the need for specific nutrients and fluid when intake may be poor8.
Fatigue and Weakness
COVID-19 may lead to muscle weakness and fatigue, impacting on a patient’s ability to undertake normal activities of daily living, such as shopping and cooking.
Isolation
Social distancing and self-isolation, due to infection with COVID-19, may impact nutritional intake e.g.:
- Poor food availability and accessibility for those who struggle to go to the shops
- Lack of visits from family or friends to provide food, company and feeding assistance
- Cancellation of social lunch clubs
Screening for malnutrition across all settings, including the community, in patients with and recovering from COVID-19, is key to maximise recovery from the illness. Use of a validated screening tool such as the Malnutrition Universal Screening Tool ('MUST') is recommended9. During the COVID-19 pandemic, healthcare professionals have had to radically change their way of working, in many cases moving to remote consultations. Identifying the risk of malnutrition usually relies on recording current weight, previous weight and height, to calculate body mass index (BMI) (step 1 of ‘MUST’) and percentage unintentional weight loss (step 2 of ‘MUST’). For people in the community during the COVID-19 pandemic, if physical measures are not possible it is recommended10:
- To use patient reported values of current weight, height, and previous weight to calculate Step 1 and Step 2 of ‘MUST’
- Where it is not possible to obtain physical or self-reported measures of weight or height there are a series of subjective criteria that can be used to form a clinical impression of an individual’s malnutrition risk category:
Subjective Criteria10
BMI
- Clinical impression – thin, acceptable weight, overweight. Obvious wasting (very thin) and obesity (very overweight) can be noted
Unplanned weight loss (particularly relevant in patients with COVID-19)
- Clothes and/or jewellery have become loose fitting
- History of decreased food intake, reduced appetite and/or dysphagia (swallowing problems) over 3-6 months, underlying disease or psycho-social/physical disabilities likely to cause weight loss.
- COVID-19 infection is very likely to cause unplanned weight loss if food intake is reduced by the effects of the disease and its management e.g. anorexia, breathlessness, impact of management options (sedation, continuous positive airway pressure (CPAP)/non-invasive ventilation (NIV), changes to taste and smell, psychological factors (e.g. anxiety), social restrictions
Acute disease
- If a patient is acutely ill with COVID-19 and is unlikely to have no nutritional intake for more than 5 days or has had no nutritional intake for more than 5 days.
Use the combination of subjective criteria to estimate a malnutrition risk category (low, medium or high) based on your overall evaluation.
The following questions can assist in obtaining information to form this clinical impression and help you select the most appropriate dietary advice resources on this website:
- How is your appetite lately? How are you managing with your eating and drinking?
- How would you describe your weight? What is a usual weight for you?
- Do you feel like your weight has changed in the last few weeks or months?
- How are your clothes and jewellery fitting? Do they feel like they fit differently to usual?
The Malnutrition Pathway COVID-19 resource finder below uses a series of prompts to assist you in choosing the information most appropriate for your patients based on either a ‘MUST’ score or appetite and weight descriptor.
Patients with COVID-19 may struggle to meet their nutritional requirements due to the presence of some or all of the nutritional challenges that can affect dietary intake (for more information see typical symptoms of COVID-19, ABOVE). A range of strategies may need to be considered to provide adequate nutrition support to people during and after COVID-19 illness.
The COVID-19 dietary advice leaflets are intended to give general advice on the optimisation of intake in those with a poor appetite and include ideas for individuals on getting the most out of their food when they are unwell. These include tips on:
- maintaining a balanced diet
- protein - which may warrant special attention due to increased needs for protein during illness and recovery12. Further information on the evidence-based guidelines for protein requirements in ageing and disease can be found in the leaflet ‘Information to help meet protein needs: A healthcare professional fact sheet’ HERE
- making the most of food via food fortification when required
- meeting vitamin and mineral requirements during illness and when appetite is poor – supplementation may be required1
- the importance of vitamin D and supplementation, particularly in those who are spending a lot of time indoors. It is recommended that adults take a supplement containing 400 international units (IU) [10 micrograms] of vitamin D per day11.
- the incorporation of oral nutritional supplements into the diet when prescribed or self-purchased
- eating when short of breath
- managing a dry mouth
- managing changes or loss in taste and smell
- getting the foods you need (including social care support)
Consideration should also be given to the ability of the patient or their carer to act on the dietary advice given, with regular monitoring built into clinical reviews. Care should be taken with food-based strategies to ensure adequate provision of protein, vitamins and minerals13.
Underlying conditions
Be alert to the presence of underlying conditions, such as diabetes which may make patients prone to severe infections of COVID-19. Erratic blood glucose levels in these patients can arise secondary to the inflammatory response and insulin resistance14. The relevance of dietary advice previously provided may need to be considered, reassessed or relaxed in the presence of a poor appetite/unintentional weight loss. Blood glucose levels should be monitored and managed to minimise the risk of systemic complications8.
Medications and insulin regimens may need to be reviewed by the diabetes team both during and after illness and if there has been a significant amount of weight loss. Equally, those on blood pressure medication may require adjustments in dose and type. Referral to speech and language therapy should be made for patients with dysphagia or swallowing difficulties.
Always use clinical judgement when using the Malnutrition Pathway COVID-19 resources in those with complex conditions which may require referral to a dietitian for specialist dietary advice.
ONS may be required in those with a medium or high risk of malnutrition especially when intake is severely impacted in the short-term such as during an infection or after a hospital admission. Good quality evidence4 shows that ONS increase intakes of energy, protein and micronutrients without suppressing appetite. ONS should be used in addition to normal diet and not as a food replacement3. CLICK HERE for further information on flavours and formats of products.
In COVID-19 it is important to consider the specific nutritional needs of the patient. The The British Dietetic Association (BDA) has developed guidance for prescribing ONS in the community, which highlights that local teams should review formularies to see if additional products need to be added that would support patients suffering/recovering from COVID-1915. MORE INFORMATION
The European Society for Parenteral and Enteral Nutrition (ESPEN) recommends giving ONS to COVID-19 patients that provide at least 400 kcal/day and ≥30g protein/day when oral intake is insufficient to meet estimated nutritional requirements1. High protein ONS may be required to achieve this, particularly amongst older patients, those with chronic conditions3, and in patients who have been discharged from an intensive care unit (ICU)16.
If there is ongoing concern regarding breathlessness, fatigue or if patients are using a mask or nebulisers regularly then a ready-to-drink, low volume ONS could be considered to reduce the time/effort needed to prepare and consume the ONS.
Ensure ONS prescription requests meet the Advisory Committee on Borderline Substances (ACBS) indications, goals have been set and arrangements are in place for review either by community dietetic services, general practitioner (GP) or other community healthcare professional.
Patients with swallowing problems may require specialised pre-thickened ONS or thickening powders. Dysphagia can affect up to a third of patients who have been cared for in intensive care and required mechanical ventilation. These patients should be assessed. GUIDANCE IS AVAILABLE if there are suspicions of dysphagia; consult a dietitian and/or a speech and language therapist.
Considerations regarding self-purchase and use of powdered ONS
A number of nutritional supplements are available for self-purchase in supermarkets, pharmacies and online. Consider how accessible these may be in the COVID-19 pandemic. Before recommending powdered ONS to patients consider the following17,18:
1. Clinical appropriateness
2. Does the patient/carer have the physical ability to make up?
3. Does the patient/carer have access to both a fridge and fresh milk?
4. Does the patient have adequate storage for milk and boxes of powder?
5. Can the patient/carer make up the powdered ONS as directed on the package to ensure safe handling practice?
If there is concern with the above, then a ready-made ONS may be more appropriate.
When to stop an ONS prescription3
Consideration of stopping an ONS prescription should be made when:
- Goals of intervention have been met
- Individual is clinically stable/acute episode has abated
- Individual is back to their normal eating and drinking pattern and is no longer at risk of malnutrition
- No further intervention would be appropriate
Additional Support - for complex patients, those at high risk of malnutrition and those who are at medium risk of malnutrition who do not improve despite preliminary intervention, consider a dietetic referral.
Patient centred goals should be discussed and agreed, including what matters to patients19, for those patients offered nutrition support, including dietary advice with or without oral nutritional supplements. It may be difficult to monitor patients if this has to be done remotely but such goals could include:
- During acute illness: minimise loss of weight/muscle mass/strength
- In recovery from illness:
- Gain muscle mass/patient feeling stronger
- Return to a desirable weight
- Resume normal hobbies
- Improve stamina e.g. ability to walk up the stairs without feeling breathless or to walk further for longer
- Achieve functional independence
Patients receiving any form of oral nutrition support should be regularly reviewed against goals set and agreed to assess progress and understand if any nutrition support strategies can be stopped or need starting. In the case of COVID-19 patients, the interval should be based on clinical judgement taking into account severity of disease and malnutrition risk; this would normally be monthly but might range from a 1-week interval to 3 months. Monitoring can include:
- Weight/BMI – self reporting of weight and height is considered reliable10
- Functional tests such as sit to stand
- Self-reported activity and ability to undertake activities of daily living
- Patient’s report of progress towards goals agreed
- Compliance to dietary advice and ONS
MALNUTRITION PATHWAY COVID-19 RESOURCE FINDER
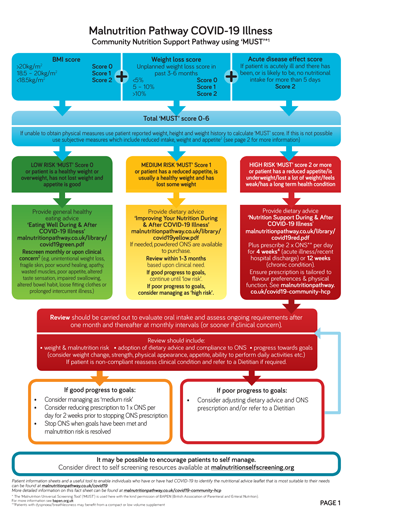
The COVID-19 Illness Community Nutrition Support Pathway aims to assist community healthcare professionals in the identification and management of patients who are at nutritional risk during or after COVID-19 illness.
Please refer to the local department of nutrition & dietetics or community dietitians where necessary
Provide ‘Eating Well During and After COVID-19 Illness’ leaflet
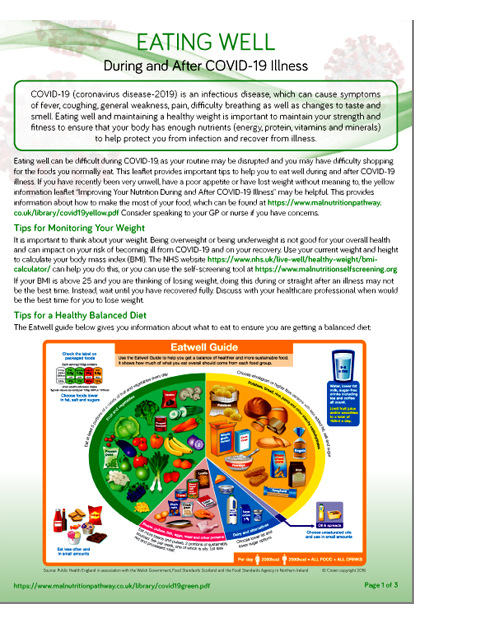
This leaflet aims raise awareness of the importance of a healthy diet, and provide advice on accessing foods during social distancing.
Provide ‘Improving Your Nutrition During and After COVID-19 Illness’ leaflet

This leaflet provides dietary advice to optimise intake and includes a range of ideas to help patients and carers achieve an adequate intake of protein, as well as energy and micronutrients, whilst helping patients to manage symptoms such as breathlessness, changes to taste and smell, weakness and fatigue.
Note: Nutritional supplements are available on prescription and for self-purchase and may be useful in addition to the diet (See section on self-purchase and powdered nutritional supplements in oral nutritional supplements section for more information)
Provide ‘Nutrition Support During and After COVID-19’ leaflet
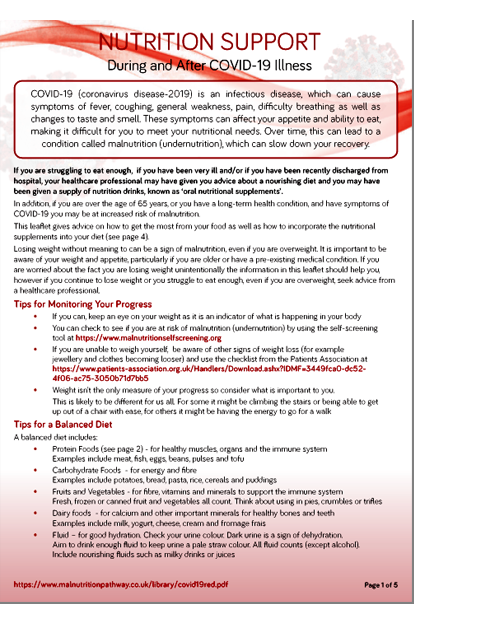
This leaflet provides dietary advice to optimise nutritional intake whilst helping patients to manage symptoms such as breathlessness, changes to taste and smell, weakness and fatigue, along with guidance to incorporate oral nutritional supplements (ONS) into the diet.
Where dietary advice is inadequate to meet nutritional requirements in those with high risk of malnutrition2 and those with COVID-191 it is recommended ONS should be prescribed. See Oral Nutritional Supplements (ONS) – When Dietary Advice is Not Enough section for further information.
For patients with COVID-19 who have required hospital admission, screening for malnutrition at the point of hospital discharge to assess their ongoing need for nutrition support at home, and review by a dietitian, is recommended to determine the need for nutritional management including the provision of and continuation of ONS on prescription1. Care should be coordinated between the acute and community settings. Local formularies should be reviewed in conjunction with the local dietetic team and Clinical Commissioning Group (CCG)/Health Board, to ensure appropriate ONS are available to support the rehabilitation of COVID-19 patients15. The European Society for Parenteral and Enteral Nutrition (ESPEN) recommends the consideration of a high protein, low volume supplement1.
Local policies for discharge of patients requiring on-going oral nutrition support in the community can still be applied but may need to be adapted to provide more bespoke guidance on managing patients recovering from a COVID-19 infection, to meet increased demand or support those where discharge is rapid.
Provide ‘Eating Well During and After COVID-19 Illness’ leaflet
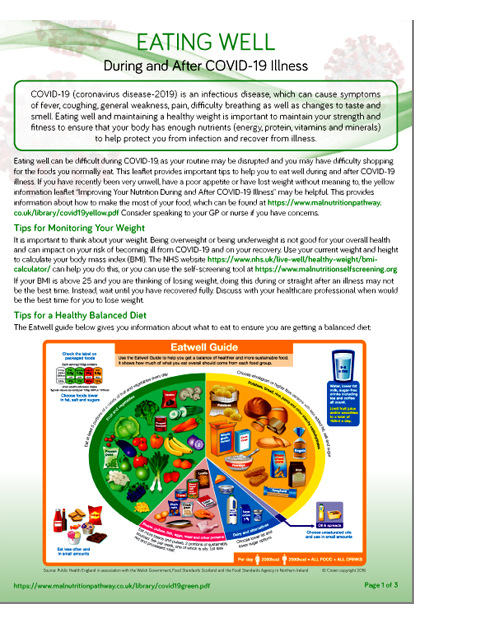
This leaflet aims raise awareness of the importance of a healthy diet, and provide advice on accessing foods during social distancing.
Patients should receive information about how to access ongoing food supplies/food deliveries especially where help from family is not available and patients need to be shielded. In some areas hospitals are providing discharge food packs, in other areas local authorities are providing support.
Provide ‘Improving Your Nutrition During and After COVID-19 Illness’ leaflet

This leaflet provides dietary advice to optimise intake and includes a range of ideas to help patients and carers achieve an adequate intake of protein, as well as energy and micronutrients, whilst helping patients to manage symptoms such as breathlessness, changes to taste and smell, weakness and fatigue.
Note: Nutritional supplements are available on prescription and for self-purchase and may be useful in addition to the diet (See section on self-purchase and powdered nutritional supplements in oral nutritional supplements section for more information)
Patients should receive information about how to access ongoing food supplies/food deliveries especially where help from family is not available and patients need to be shielded. In some areas hospitals are providing discharge food packs, in other areas local authorities are providing support.
Provide ‘Nutrition Support During and After COVID-19’ leaflet
This leaflet provides dietary advice to optimise nutritional intake whilst helping patients to manage symptoms such as breathlessness, changes to taste and smell, weakness and fatigue, along with guidance to incorporate oral nutritional supplements (ONS) into the diet.
Where dietary advice is inadequate to meet nutritional requirements in those with high risk of malnutrition2 and those with COVID-191 it is recommended ONS should be prescribed. See Oral Nutritional Supplements (ONS) – When Dietary Advice is Not Enough section.
Patients should receive information about how to access ongoing food supplies/food deliveries especially where help from family is not available and patients need to be shielded. In some areas hospitals are providing discharge food packs, in other areas local authorities are providing support.
For those who required critical care, long-term nutritional problems can persist after hospital discharge including:
- Prolonged hypermetabolism and catabolism (muscle breakdown)20
- Poor appetite16, 21-23 lasting around 3 months21
- Dysphagia, affecting around 50% of patients post-extubation and taking up to 3-6 months to recover24
- Frailty24 and ICU-acquired weakness (ICUAW), characterised by loss of muscle mass and strength, occurring in approximately 46% of patients25 and lasting up to 2 years following ICU discharge26
Tailored nutritional management is recommended for patients recovering from ICU after hospital discharge. Individuals should remain under the care of either the hospital or community healthcare team who can provide advice on recovery. If this has not been provided it is suggested the hospital or community dietetic department is contacted for further advice. Other specialist services, such as psychology and physiotherapy, may be required for patients recovering from ICU. Refer to local pathways/policy.
 The Nutrition Support During and After COVID-19 leaflet may be helpful but should not over-ride advice from your hospital rehabilitation team or dietitian.
The Nutrition Support During and After COVID-19 leaflet may be helpful but should not over-ride advice from your hospital rehabilitation team or dietitian.
If the individual is not under the care of any specific team it is suggested the local dietetic department is contacted for further advice.
The BDA Critical Care Specialist Group has produced specific advice for patients further to crictical illness - https://www.bda.uk.com/resource/nutrition-at-home-after-critical-illness.html
Patients should receive information about how to access ongoing food supplies/food deliveries especially where help from family is not available and patients need to be shielded. In some areas hospitals are providing discharge food packs, in other areas local authorities are providing support.
A number of professional organisations have produced resources for healthcare professionals in relation to nutrition and COVID-19. These are based on expert consensus and are being updated as the crisis evolves. FURTHER INFORMATION
References
1. Barazzoni R et al, endorsed by the ESPEN Council. ESPEN expert statements and practical guidance for nutritional management of individuals with sars-cov-2 infection, Clinical Nutrition. 2020. https://doi.org/10.1016/j.clnu.2020.03.022.
2.European Centre for Disease Prevention and Control. Rapid Risk Assessment: Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK – eighth update. 2020. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-eighth-update-8-april-2020.pdf Accessed 27/05/20
3.Holdoway et al. A Guide to Managing Adult Malnutrition in the Community. 2017. https://www.malnutritionpathway.co.uk/library/managing_malnutrition.pdf Accessed 27/05/20
4.Stratton RJ et al. Disease-related malnutrition: an evidence-based approach to treatment. Oxford: CABI publishing. 2003
5.British Lung Foundation. Eating well with a lung condition. How can food affect my symptoms? https://www.blf.org.uk/support-for-you/eating-well/diet-and-my-symptoms Accessed 27/05/20
6.Xydakis MS et al. Smell and taste dysfunction in patients with COVID-19. The Lancet: Infectious Diseases. 15 April 2020. https://doi.org/10.1016/S1473-3099(20)30293-0 Accessed 27/05/20
7.NHS. Symptoms and what to do - Coronavirus (COVID-19). 2020. https://www.nhs.uk/conditions/coronavirus-covid-19/symptoms-and-what-to-do/ Accessed 27/05/20
8.Gandy J [Ed]. Manual of Dietetic Practice 6th Edition. 2019. Wiley-Blackwell: London.
9.Elia M. The “MUST” report. Nutritional screening for adults: a multidisciplinary responsibility. BAPEN: Redditch, UK. 2003. https://www.bapen.org.uk/pdfs/must/must-report.pdf Accessed 27/05/20.
10.British Association of Parenteral and Enteral Nutrition (BAPEN). Practical guidance for using ‘MUST’ to identify malnutrition during the COVID-19 pandemic: Malnutrition Action Group (MAG) update. May 2020 https://www.bapen.org.uk/pdfs/covid-19/covid-mag-update-may-2020.pdf Accessed 27/05/20
11.National Institute for Health and Care Excellence (NICE). Vitamin D deficiency in adults - treatment and prevention. 2018 https://cks.nice.org.uk/vitamin-d-deficiency-in-adults-treatment-and-prevention#!topicSummary Accessed 27/05/20
12.Deutz NE et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clinical Nutrition. 2014; 33: 929-936.
13.National Institute for Health and Care Excellence (NICE). Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition [Clinical Guideline 32]. 2006. NICE. https://www.nice.org.uk/guidance/cg32 Accessed 27/05/20
14.Puig-Domingo M et al. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020; 68: 2-5.
15.British Dietetic Association (BDA). Top tips for prescribing Oral Nutritional Supplements and Enteral Feeds in the community for Adults and Paediatrics. https://www.bda.uk.com/resource/top-tips-for-prescribing-oral-nutritional-supplements-and-enteral-feeds-in-the-community-for-adults-and-paediatrics.html Accessed 27/05/20
16.Zanten ARH et al. Nutrition therapy and critical illness: practical guidance for the ICU, post-ICU, and long-term convalescence phases. Critical Care. 2019; 23: 368. doi: 10.1186/s13054-019-2657-5.
17.British Dietetic Association (BDA). Practical considerations for nutritional management of non-ICU COVID-19 patients in hospital. 2020. https://www.bda.uk.com/resource/practical-considerations-for-nutritional-management-of-non-icu-covid-19-patients-in-hospital.html Accessed 27/05/20
18.Mulholland P, McKnight E, Prosser J. Audit of compliance with NI formulary for oral nutritional supplements in South Eastern Trust. Clinical Nutrition ESPEN. 2019; 29: 282–283 https://clinicalnutritionespen.com/article/S2405-4577(18)30716-2/pdf Accessed 27/05/20
19.NHS England. Universal Personalised Care. Implementing the Comprehensive Model. 2019 https://www.england.nhs.uk/wp-content/uploads/2019/01/universal-personalised-care.pdf
20.Wischmeyer PE. Tailoring nutrition therapy to illness and recovery. Crit Care. 2017; 21 (3): 316.
21.Merriweather JL et al. Appetite during the recovery phase of critical illness: a cohort study. European Journal of Clinical Nutrition. 2018; 72: 986–992.
22.Merriweather JL et al. Nutritional Care After Critical Illness: A Qualitative Study of Patients Experiences. Journal of Human Nutrition and Dietetics. 2016 Apr;29(2):127-36.
23.Helliwell V et al. Failure to regain weight after critical illness: a short review. ICU Management. 2006; 6 (4),18.
24.Singer et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clinical Nutrition. 2019; 38 (1): 48-79.
25.Stevens RD et al. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Medicine. 2007; 33: 1876–1891.
26.Hermans G & Van den Berghe G. Clinical review: intensive care unit acquired weakness. Critical Care. 2015; 19:274. doi: 10.1186/s13054-015-0993-7.
Other useful resources for healthcare professionals
Useful nutritional and dietary resources for DIETITIANS, PHARMACISTS, NURSES, GENERAL PRACTITIONERS and SPEECH & LANGUAGE THERAPISTS MORE
RESOURCES FOR HEALTHCARE PROFESSIONALS
 NEW: Good Nutritional Care: COVID-19
NEW: Good Nutritional Care: COVID-19
‘Why Good Nutritional Care is Important During and After COVID-19 Illness’.
Includes advice for care home staff on dealing with symptoms that may affect the nutritional intake of residents during and after COVID-19 infection.
Further Information
We can be contacted regarding the malnutrition pathway materials and website
COVID-19 & Good Nutrition: Patient and Carer Resources
An overview with useful resources for patients and carers. Endorsed by the British Dietetic Association (BDA), the Royal College of Nursing (RCN) and the British Association of Parenteral and Enteral Nutrition (BAPEN) MORE
COVID-19: Resources for Healthcare Professionals
Endorsed by the British Dietetic Association (BDA), the Royal College of Nursing (RCN) and the British Association of Parenteral and Enteral Nutrition (BAPEN) MORE