 Managing Adult Malnutrition
Managing Adult Malnutrition
Including a pathway for the appropriate use of
oral nutritional supplements (ONS)
News
From time to time we will publish relevant news articles on this section of the website. News and updates regarding the management of adult malnutrition in the community are published throughout the year in our PATHWAY NEWSLETTER
MALNUTRITION PATHWAY LAUNCHES NEW MICROSITE FOR THE PRIMARY CARE NETWORK (PCN) TEAM
The Malnutrition Pathway has launched a NEW MICROSITE which includes sections aimed at different members of the PCN team. It provides guidance on the identification and management of malnutrition along with advice on when to refer on to other appropriate healthcare professions. The sub sections include information aimed at:
DIETITIANS including materials to assist Dietitians in the training other members of the PCN team in the identification and management of malnutrition.
GENERAL PRACTITIONERS and PRACTICE NURSES including advice on screening, treatment, prevention, management and monitoring.
PHYSICIAN ASSOCIATES , NURSE ASSOCIATES & TRAINEES and PARAMEDICS with advice on identifying those at risk of malnutrition, carrying out screening and assessment, giving nutritional advice, and referring on to an appropriate healthcare professional for more detailed assessment.
PRACTICE/CLINICAL PHARMACISTS , COMMUNITY PHARMACISTS and PHARMACY TECHNICIANS , with advice on incorporating screening, management and monitoring of ONS prescriptions.
PHYSIOTHERAPISTS and OCCUPATIONAL THERAPISTS with advice on identifying malnutrition in high-risk patient groups who they see regularly, including the frail elderly and those with long term conditions.
CARE CO-ORDINATORS , HEALTH & WELLBEING COACHES and SOCIAL PRESCRIBERS , including links to key resources that may be of use to individuals who are having difficulty with eating and drink.A number of new factsheets are also available on the new PCN microsite which are linked to the specific pages including:
- Advice on initiating conversations about (unintentional) weight loss and diet – FACTSHEET
- Subjective indicators of malnutrition risk – FACTSHEET
- Symptoms and problems that may be affecting a person’s ability to eat and drink – FACTSHEET
- Considerations when prescribing oral nutritional supplements for those at high risk of malnutrition - FACTSHEET
Previous news items
-
THE IMPORTANT ROLE DIETITIANS PLAY IN TACKLING MALNUTRITION: RAISING AWARENESS
RAISING AWARENESS OF THE IMPORTANT ROLE DIETITIANS PLAY IN TACKLING MALNUTRITION IN THE COMMUNITY
 As part of our Malnutrition Awareness Week activities (10-16 October 2022) the Malnutrition Pathway has this month been working with Dietitians across the country to raise awareness of disease-related malnutrition and the important role that Dietitians play in identifying and treating it. Dietitians from across England, Wales and Scotland have worked with Paul Pennington from WORD ON HEALTH to develop interviews which focus on the role that Dietitians play in the community.
As part of our Malnutrition Awareness Week activities (10-16 October 2022) the Malnutrition Pathway has this month been working with Dietitians across the country to raise awareness of disease-related malnutrition and the important role that Dietitians play in identifying and treating it. Dietitians from across England, Wales and Scotland have worked with Paul Pennington from WORD ON HEALTH to develop interviews which focus on the role that Dietitians play in the community.Thank you to ‘Word on Health’ and all the Dietitians involved who have given up their personal time to be involved in this initiative and to help inform the general public about what Dietitians do, what malnutrition is and what to do if they are concerned about unintentional weight loss. You can listen to the ‘Word on Health’ interview HERE
A selection of some of the amazing interviews given can be found at the links below:
- SCOTLAND
- Dalhia Campbell Tayside | Claire Livie Dundee | Gordon McAndrew Ayrshire
- WALES
- Karen Voas-Wootton North Wales | Lucy Marland Cardiff
- SOUTH WEST ENGLAND
- Ruth Harvey Teignmouth | Jennifer Van-Zant Isle of Wight
- WEST MIDLANDS
- Victoria Dagnan Dudley & Netherton | Kayennat Toofany Brierley Hill & Amblecote
- YORKSHIRE
- Nusrat Kausar Bradford | Clara Carr South West Yorkshire | Kwayera Simpson West Yorkshire
- LONDON Joe Alvarez Hackney | Neil McCreanor North London
-
TEN YEARS OF TACKLING MALNUTRITION IN THE COMMUNITY
TEN YEARS OF TACKLING MALNUTRITION IN THE COMMUNITY
This year marks the 10th Anniversary of the launch of the Managing Adult Malnutrition in the Community guidance. Since its launch by a multi-disciplinary consensus panel in 2012, the Malnutrition Pathway website (www.malnutritionpathway.co.uk) has received nearly a quarter of a million visits. In the past year alone the website has been visited by over 30,000 professionals, patients and carers from over 150 countries around the world. Over 60,000 copies of the Managing Adult Malnutrition in the Community document and nearly 16,000 of the corresponding patient leaflets were downloaded in 2021. Year on year growth in visits and downloads, reflects the ongoing need for guidance and resources to help support the 3 million people in the UK who are at risk of malnutrition, 93% of whom live in the community1.
The guidance document was developed to assist non-nutrition experts in the identification, treatment and prevention of disease related malnutrition in the community. Now in its third iteration the Managing Adult Malnutrition in the Community document has received consistent endorsement from ten professional and patient organisations and includes an endorsement statement from the National Institute for Health and Care Excellence (NICE)2.
The resources are accessed by a broad range of healthcare professionals in the community, including Dietitians, Nurses, GPs, Pharmacists, Physiotherapists, Speech and Language Therapists, Healthcare Assistants and Care Homes Personnel to support the identification, treatment and prevention of disease-related malnutrition. Pilot studies have demonstrated a positive impact on patient outcomes and a reduction in healthcare usage through better nutrition3,4.
Feedback from end-users over the past ten years has facilitated the creation of additional materials including patient and carer leaflets and new resources focusing on key areas in clinical nutrition such as COPD, COVID-19, cancer and sarcopenia. The website now hosts sections dedicated to specific healthcare professional groups involved in the care of patients at risk of malnutrition. A patient and carer section enables care professionals and patients and family members to easily access resources relevant to them.
“Advancing age and the presence of an acute illness or long-term condition can have a profound impact on appetite, absorption of nutrients and the ability to source food, prepare meals and consume enough to maintain nutritional status, predisposing an individual to the deleterious effects of malnutrition. Given that health and social care costs for individuals with malnutrition are three to four times more than managing a nourished individual,5 it is crucial that nutritional screening and nutritional care is embedded into clinical care pathways to identify and treat those at risk of malnutrition at the earliest opportunity” says Dr Anne Holdoway, chair of the Malnutrition Pathway panel. “The expertise of Dietitians in assessing patients with nutritional issues and providing bespoke advice is not to be underestimated but as a relatively small workforce we cannot currently treat everyone. Transferring knowledge and skills and providing tools and resources to empower members of the healthcare team to look for malnutrition, especially in those at increased risk, enables early action to be taken to improve healthcare outcomes and manage costs. This was the driving force behind the development of the managing adult malnutrition in the community pathway and resources. It has been hugely rewarding to see that 10 years on, the resource and its updates remain as relevant as when they were initially launched and thus continue to help the health and social care teams provide nutritional care and advice to some of our most vulnerable individuals.”
NOTES
- Groups at high risk of malnutrition include older people, those recently discharged from hospital, those with chronic disease, progressive neurological disease, acute illness, frailty, undergoing rehabilitation or receiving end of life or palliative care.
- The clinical consequences of malnutrition include impaired immune response, reduced muscle strength, impaired wound healing and increased falls. Malnourished individuals have more hospital admissions/readmissions, longer length of hospital stay and greater primary care healthcare needs, therefore identification and management is key
- Production of the Managing Adult Malnutrition in the Community materials has been made possible by an unrestricted educational grant from Nutricia
References
- Elia M and Russell CA. Combating Malnutrition: Recommendations for Action. Report from the advisory group on malnutrition, led by BAPEN. 2009
- The ‘Managing Adult Malnutrition in the Community’ document and supporting patient materials have been supported by 10 key professional and patient associations:
- •The British Association For Parenteral And Enteral Nutrition (BAPEN)
- •The British Dietetic Association (BDA)
- •The British Pharmaceutical Nutrition Group (BPNG)
- •The National Nurses Nutrition Group (NNNG)
- •The Patients Association
- •The Primary Care Society for Gastroenterology (PCSG)
- •The Primary Care Pharmacy Association (PCPA)
- •The Royal College Of General Practitioners (RCGP)
- •The Royal College Of Nursing (RCN)
- •The Royal Pharmaceutical Society (RPS)
In addition the guidance also includes the following NICE endorsement statement:
This booklet supports the implementation of recommendations in the NICE guideline on nutrition support for adults. It also supports statements 1, 2 and 5 in the NICE quality standard for nutrition support in adults. National Institute for Health and Care Excellence Endorsed December 2017. Updated June 2021 - Brown F et al (2020) Economic impact of implementing malnutrition screening and nutritional management in older adults in general practice. J Nutr Health Aging 24(3):305–311
- Cawood A et al (2017) Local implementation of a pathway to manage malnourished COPD patients in the community. Eur Respir J 50 (suppl 61): PA1609
- Elia M, on behalf of the Malnutrition Action Group (BAPEN) and the National Institute for Health Research Southampton Biomedical Research Centre. The cost of malnutrition in England and potential cost savings from nutritional interventions (full report). 2015.
-
NEW RESOURCES: OPTIMISING THE NUTRITIONAL CARE OF PATIENTS WITH CANCER
NEW ONLINE RESOURCE TO ASSIST HEALTHCARE PROFESSIONALS IN OPTIMISING THE NUTRITIONAL CARE OF PATIENTS WITH CANCER
The Malnutrition Pathway has developed a NEW ONLINE RESOURCE focusing on optimising the nutritional care of patients with cancer . Developed in conjunction with Mhairi Donald, Consultant Oncology Dietitian and Dr Anne Holdoway, Consultant Dietitian, the resource aims to enable health and care professionals to recognise nutritional issues and provide first line advice supported by downloadable patient fact sheets. It has been developed in response to a growing desire amongst patients and carers for information on diet and nutrition in cancer1,2 and includes specific information on dealing with common nutrition impact symptoms.
The new resource outlines the impact of malnutrition in cancer, advises on nutrition screening and assessment and gives advice for both healthcare professionals and patients on ways to adjust the diet to prevent or manage common nutrition impact symptoms. It also includes information on diet in the prehabilitation phase prior to treatment, top line information on nutrition support and diet therapy, the use of oral nutritional supplements when indicated, and includes a summarised step by step guide.
Nutrition is considered highly important by cancer patients across their trajectory of care, from the period of diagnosis through treatment and beyond into survivorship and in palliation. Many patients will experience diet-related issues throughout the journey which can persist well beyond the treatment phase1. These issues not only contribute to the development of malnutrition but create distress and add to existing anxieties. In addition, disease-related malnutrition, cachexia and sarcopenia (loss of muscle) result in poorer outcomes and increased mortality, hence where possible should be prevented, identified and treated3.
An estimated 1 in 3 patients with cancer attending out-patients are at nutritional risk4 and up to 83&%; of patients experience malnutrition during the course of their disease depending on the type of cancer, treatment and nutritional assessment method used5-8.
Nutritional risk is associated with a number of common clinical issues (e.g. fatigue, anorexia, gastrointestinal symptoms, sore mouth). These issues are usually noted and recorded but importantly should act as an indicator for the healthcare team that further nutritional assessment may be warranted, triggering a referral for more detailed assessment by a dietitian or nutrition team4.
‘Nutritional issues and poor nutritional status can result from the local effects of the cancer itself, the metabolic response to the cancer, and the treatments used such as chemotherapy, radiotherapy, immunotherapy and surgery’ says Mhairi Donald, Consultant Oncology Dietitian. ‘All of these can have immediate short-term effects, as well as longer-term effects, limiting the ability to eat and drink. It is therefore important that we seek to optimise the nutritional status of patients at diagnosis, during prehabilitation, treatment and rehabilitation.’
‘Timely nutritional interventions can improve nutritional status, body composition, function, symptoms, quality of life, the patient experience and ultimately survival. Despite this the provision of appropriate nutritional care can be delayed, and in some cases overlooked, adding diet-related anxiety to anxieties that already exist amongst patients and their families’ says Dr Anne Holdoway, Chair of the Malnutrition Pathway panel. ‘The new resources developed by the Malnutrition Pathway aim to support healthcare professionals in identifying the common symptoms and issues interfering with the ability to eat and drink amongst those living with cancer, provide patients with appropriate advice to alleviate the issues and ultimately enhance the overall patient experience and improve clinical outcomes.’
‘There are many reasons why a head and neck cancer patient is likely to experience malnourishment. Prior to treatment a patient may simply not eat enough due to a physical obstruction, or pain caused from an untreated tumour’ says Michelle Vickers, CEO of the Head & Neck Cancer Foundation. ‘Post-operatively patients may suffer from issues with oral pain, discomfort, mechanical function and dry mouth. Malnutrition can therefore develop as a direct result from the physical impacts of surgery and ongoing oncology treatment. This often becomes a problem and effects areas such as chewing, swallowing, saliva production and taste. We fully support this valuable piece of work as it will help our patients cope in this vital area. A common concern for patients, family and friends in our support group is food and drink. What to cook, how to eat it, how to enjoy it and how to get the best from it. The ability to eat properly and the importance of a nourishing diet are certainly taken for granted.’
The ‘Optimising Nutritional Care in Cancer’ web resource is available free to access:
A number of patient information sheets provide top tips on managing nutrition impact symptoms such as reduced appetite, dry mouth, taste changes, swallowing issues, altered bowel habit and fatigue, as well as a fact sheet focusing on getting ready for treatment (prehabilitation). All are free to download within the resource.
Production of the cancer resource materials has been made possible by an unrestricted educational grant from Nutricia.
Further information on the Head & Neck Cancer Foundation can be found at HNCF.org.uk
References
- Sullivan ES et al, A national survey of oncology survivors examining nutrition attitudes, problems and behaviours, and access to dietetic care throughout the cancer journey. Clinical Nutrition ESPEN. 2021; 41: 331-339.
- European Cancer Patient Coalition. Living well during cancer treatment. Addressing cancer patients concerns: series I out of II. 2019. https://ecpc.org/wp-content/uploads/2020/01/ecpc-nutrition-booklet-living-well-during-cancer-treatment-EN.pdf
- Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. European Journal of Oncology Nursing 2005;9:S51–S63. Suppl 2:S51-63.
- Bozzetti F, Mariani L, Vullo SL et al. The nutritional risk in oncology: a study of 1453 cancer outpatients. Support Care Cancer 2012;20(8):1919-1928.
- Isenring EA, Bauer JD, Capra S. The scored Patient-generated Subjective Global Assessment (PG-SGA) and its association with quality of life in ambulatory patients receiving radiotherapy. European Journal of Clinician Nutrition 2003;57:305–309.
- Better care through better nutrition: value and effects of medical nutrition - A summary of the evidence base” 2018. https://medicalnutritionindustry.com/files/user_upload/documents/medical_nutrition/2018_MNI_Dossier_Final_web.pdf
- Ravasco P. Nutrition in Cancer Patients. J Clin Med 2019; 8:1211.
- Tong H, Isenring E, Yates P. The prevalence of nutrition impact symptoms and their relationship to quality of life and clinical outcomes in medical oncology patients. Support Care Cancer 2009;17:83–90.
- Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. European Journal of Clinical Nutrition 2002;56:779–785.
Archived
-
Evidence based management of disease related malnutrition
EVIDENCE BASED MANAGEMENT OF DISEASE RELATED MALNUTRITION
UPDATED GUIDANCE INCLUDING A FOUR STEP APPROACH
The Managing Adult Malnutrition in the Community panel has updated its guidance for community healthcare professionals. The updated guide reflects the latest evidence and best practice and is encouraging professionals to consider a four step approach to the management of disease-related malnutrition:
- • Step 1: Identification of malnutrition: nutrition screening
- • Step 2: Assessment: identifying the underlying cause of malnutrition
- • Step 3: Management: identifying treatment goals and optimising nutritional intake
- • Step 4: Monitoring the intervention
Developed by a multi-professional panel with an expertise and interest in malnutrition, the evidence-based document has been updated to incorporate the most up-to-date national and international guidance as well as high quality, peer reviewed research. It emphasises the role of the multi-disciplinary team in identifying and managing malnutrition, working alongside dietitians, and provides information for non-nutrition experts on actions to optimise dietary intake along with appropriate prescribing of oral nutritional supplements (ONS) when required.
Three patient leaflets accompany the guidance document. The document and leaflets have been endorsed by ten key professional and patient organisations including the British Dietetic Association (BDA), The British Association for Parenteral and Enteral Nutrition (BAPEN), the Royal College of Nursing (RCN), the Royal College of General Practitioners (RCGP), the Royal Pharmaceutical Society (RPS) and the Patients Association1.
The clinical consequences of malnutrition can be profound. Studies have repeatedly demonstrated that undetected and untreated malnutrition reduces muscle strength, contributes to frailty, increases falls risk, slows recovery from illness and surgery, impairs psycho-social function, immune response and wound healing, all of which are associated with poorer clinical outcomes2-6. The cost of malnutrition in the UK exceeds £23.5 billion per annum6. At an individual level, a malnourished patient costs three times more to manage than a non-malnourished individual (£7,408 versus £2,155)7. Action to detect, treat and prevent malnutrition are therefore justified on both a clinical and cost basis.
Groups most at risk of malnutrition include those with chronic disease, progressive neurological disease, frailty, neuro-disability, swallowing difficulties, acute illness and those with end of life/palliative care needs. Patients undergoing prehabilitation and rehabilitation, prior to and after surgery, are also at risk and it is important that their nutritional status is optimised to prepare them for surgery and assist in their recovery. The needs of obese individuals in whom a high body mass index can mask malnutrition and sarcopenia (a loss of muscle mass and strength) should also be given special consideration.
What the experts say
“This updated guidance aims to raise awareness amongst community healthcare professionals of how the underlying causes of malnutrition may be alleviated to break the repeated cycles of malnutrition, particularly amongst those with long-term conditions.” says Dr Anne Holdoway, Consultant Dietitian and Chair of the Managing Adult Malnutrition in the Community panel. “Identifying the causes and symptoms which are interfering with a patient’s ability to eat and drink and addressing those that can be reversed or modified, needs to be an integral part of the patient’s treatment plan. Such plans also need to consider the person’s ability to act on the advice given and mitigate for any barriers either clinical, practical or social, that may affect adherence to dietary advice and, if prescribed, the choice and type of oral nutritional supplements. I hope this guidance will assist professionals in taking action early, know when to refer on to a Dietitian, and ultimately take us one step closer to optimising nutritional care for all our patients.”
“Unintentional weight loss is a red flag and may need a 2 week wait referral” says Dr Anita Nathan, GP member of the Managing Adult Malnutrition in the Community panel. “Whilst malnutrition will most frequently occur in those who are underweight, the malnutrition of our overweight and obese patients can be overlooked. It is hoped that by encouraging community healthcare professionals to implement appropriate screening, including observations such as unintentional weight loss and poor appetite or impaired swallow, with further assessment of such issues, we can aim to ensure the at-risk patients don’t slip through the net.”
“There are around 3 million people at any time in the UK who are malnourished or at risk of malnutrition” says Liz Anderson, RN, Lead Nurse for Nutrition at Buckinghamshire Healthcare NHS Trust and member of the Managing Adult in the Community panel. “Taking early action through screening and being aware of those at risk can prevent the escalating health and social care costs associated with a deteriorating state of nutrition. I hope that this four step guidance will help community healthcare professionals to confidently take relevant actions whilst also identifying those patients who need to be referred on to a Dietitian for additional support.”
“The symptoms of malnutrition share similarities with side effects of medications , in addition the metabolism of drugs is affected by body mass and physiological status” says Sam Cudby, Practice Pharmacist member of the Managing Adult Malnutrition in the Community panel “Pharmacists are in an excellent position to deliver the first tier of malnutrition management. It is important that we work as part of the multi-disciplinary team and seek guidance from our dietetic colleagues before amending prescriptions that have been recommended following a comprehensive nutritional assessment. It is hoped this evidence-based guidance will assist pharmacists in integrating nutrition screening into polypharmacy reviews to identify malnutrition, gain a more holistic view of patient’s health needs and achieve better outcomes.”
“This resource gives useful guidance for the whole multi-disciplinary team on the identification and management of malnutrition” says Dr Graham Stretch, PCPA President and PCN Clinical Director. “It is evident that the nutritional status of patients has a direct effect on their outcomes. With a spotlight on the nation’s health post-COVID, nutrition should become front and centre of care. The formation of PCNs has allowed groups of practices healthcare professionals with specialist skills as members of their team and I would encourage PCN Directors to read this guidance and consider the benefits of engaging a Dietitian as part of that multi-disciplinary team to ensure that nutritional care becomes an integral part of patient care pathways.”
Managing Adult Malnutrition in the Community
The first edition of the ‘Managing Adult Malnutrition in the Community’ guidance was launched in 2012 and it complements the ‘Managing Malnutrition in COPD’ guidelines and ‘A Community Healthcare Professional Guide to the Nutritional Management of Patients During and After COVID-19 Illness’.
The document is based on clinical experience and evidence alongside accepted best practice. A full free copy of the guide can be downloaded HERE
Patient and Carer leaflets
The guidance is accompanied by three complementary colour-coded leaflets for use by patients and their carers which have been updated to ensure they support the cultural diversity of patients. The three leaflets are:
- Nutrition Drinks (known as Oral Nutritional Supplements) – red leaflet for those at high risk of malnutrition. This leaflet outlines to patients why they have been prescribed oral nutritional supplements and offers them general advice on getting the most from their supplements, for example advice on cooking with supplements and storage
- Your Guide to Making the Most of Your Food – yellow leaflet for those at medium risk of malnutrition, which provides some simple ideas for patients on how they can get the most nutrition from the food they are eating
- Eating Well – green leaflet for those at low risk of malnutrition, gives patients advice on how to eat well and keep as healthy as possible
All three leaflets can be downloaded for free HERE
Production of the ‘Managing Adult Malnutrition in the Community’ materials was made possible by an unrestricted educational grant from Nutricia.
Further information
Please contact the Malnutrition Pathway
References
- The ‘Managing Adult Malnutrition in the Community’ document and supporting patient materials have been supported by 10 key professional and patient associations:
- The British Association For Parenteral And Enteral Nutrition (BAPEN)
- The British Dietetic Association (BDA)
- The British Pharmaceutical Nutrition Group (BPNG)
- The National Nurses Nutrition Group (NNNG)
- The Patients Association
- The Primary Care Society for Gastroenterology (PCSG)
- The Primary Care Pharmacy Association (PCPA)
- The Royal College Of General Practitioners (RCGP)
- The Royal College Of Nursing (RCN)
- The Royal Pharmaceutical Society (RPS)
This booklet supports the implementation of recommendations in the NICE guideline on nutrition support for adults. It also supports statements 1, 2 and 5 in the NICE quality standard for nutrition support in adults. National Institute for Health and Care Excellence
Endorsed December 2017. Updated June 2021 - Stratton RJ et al. Disease-related malnutrition: an evidence-based approach to treatment. Oxford: CABI publishing; 2003.
- Gossier S, Guyonnet S and Volkert D. The Role of Nutrition in Frailty: An Overview. The Journal of Frailty & Aging. 2016; 5(2)
- JAMDA. Frailty Consensus: A Call To Action. 2013; 14: 391-397
- Brotherton, Simmonds and Stroud on behalf of BAPEN Malnutrition Matters. Meeting quality standards in nutritional care. 2010. UK: BAPEN
- Meijers et al Predicting falls in elderly receiving home care: The role of malnutrition and impaired mobility, Journal of Nutrition, Health and Aging. 2012; 16(7): 654-658
- Stratton R, Smith T, Gabe S. Managing malnutrition to improve lives and save money. BAPEN. October 2018.
- Elia M, on behalf of the Malnutrition Action Group (BAPEN) and the National Institute for Health Research Southampton Biomedical Research Centre. The cost of malnutrition in England and potential cost savings from nutritional interventions (full report). 2015. http://www.bapen.org.uk/pdfs/economic-report-full.pdf
-
Patients with sarcopenia
PATIENTS WITH SARCOPENIA: Malnutrition Pathway launches new factsheet
In light of the increasing evidence on the importance of preserving muscle mass as we age1 the Malnutrition Pathway (www.malnutritionpathway.co.uk) has developed a new fact sheet focusing on sarcopenia (loss of muscle mass).
Written by Consultant Dietitians Dr Ann Ashworth and Dr Anne Holdoway, the new sarcopenia fact sheet outlines why it is important to identify sarcopenia in all patients whether they are underweight, normal weight, overweight or obese. It summarises the multiple factors that can contribute to sarcopenia and the potential consequences to health, giving practical advice on diagnosis and treatment according to the patients’ current nutritional status.
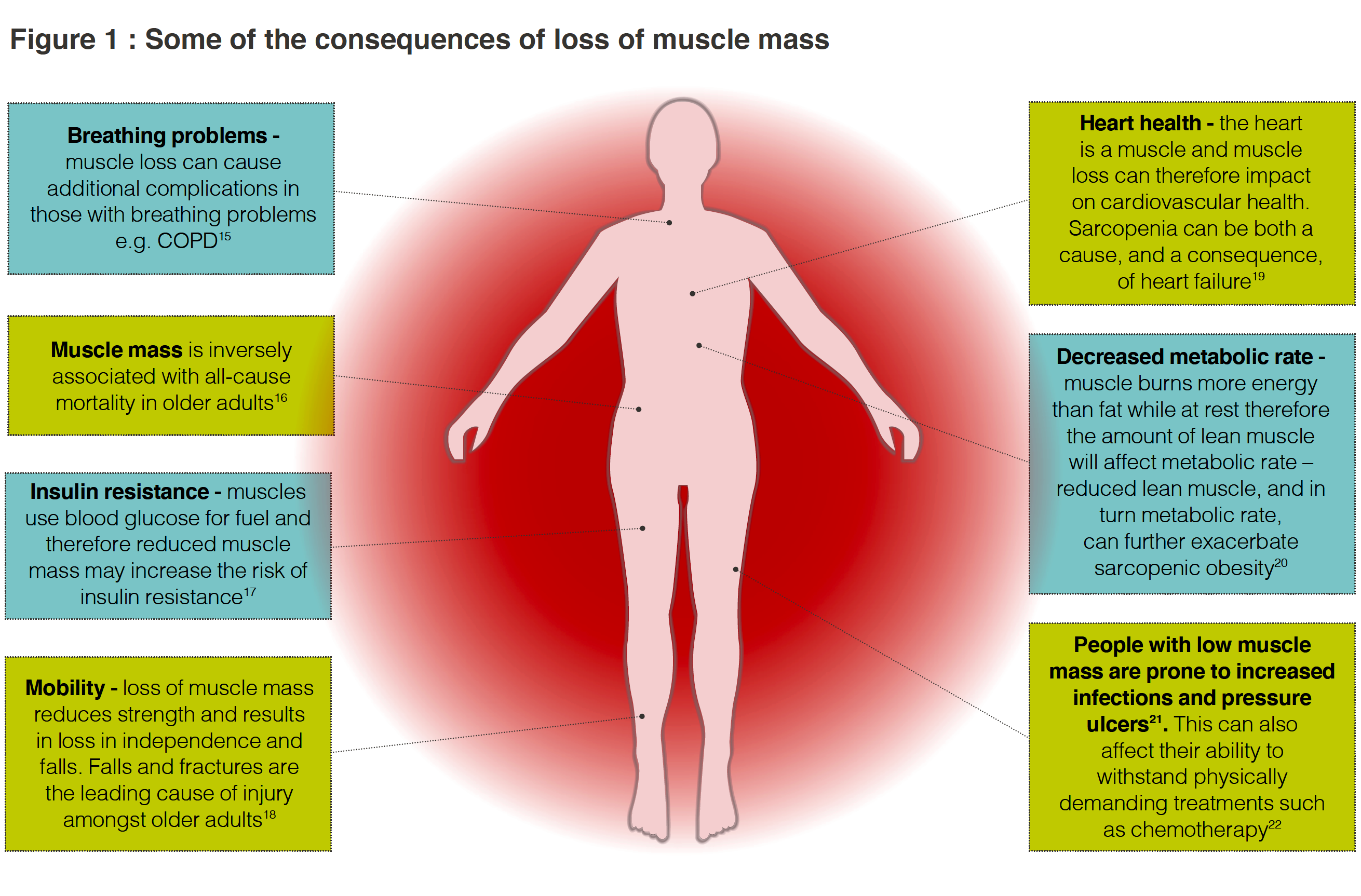
Disease, inactivity and poor nutrition can all contribute to sarcopenia and whilst it is more common in older age it can also occur in earlier life2. Left untreated, sarcopenia can affect recovery from surgery or injury3 hamper response to treatment4, reduce functional capacity5,6 or contribute to a more rapid deterioration in pre-existing conditions5-7 (see Figure 1, below).
The fact sheet gives advice on how to identify sarcopenia and malnutrition, detailing the principles of management of malnutrition and sarcopenia, including guidance on optimising nutritional intake, through diet and the inclusion of oral nutritional supplements when indicated, in combination with exercise.
"The COVID pandemic has further emphasised the impact of low muscle mass and muscle loss in impeding recovery" says Dr Anne Holdoway, Chair of the Malnutrition Pathway panel. "The combination of illness, reduced activity or bed rest, a poor appetite and reduced food intake, frequently results in weight loss particularly amongst older people and those with chronic conditions. Muscle is often lost at a disproportionate rate to fat mass. For optimal recovery, it’s important we get the message out to healthcare professionals, patients and carers about the importance of a protein rich diet, combined with resistance type exercise or activity tailored to the individual, to ensure muscle is repleted and a return to pre-illness function is achieved or improved."
"The consequences of not identifying and treating the sarcopenia can cause long term adverse outcomes for patients whilst putting additional pressure on the health service" says Dr Ann Ashworth, Malnutrition Pathway Consultant Dietitian "Whilst in malnourished patients the presence of sarcopenia may be visually obvious it is not always easy to identify sarcopenia in overweight or obese patients where it is easily missed. We hope this fact sheet will assist healthcare professionals in identify and managing sarcopenia."
The 'SARCOPENIA: LOSS OF MUSCLE MASS' fact sheet is available free to healthcare professionals and can be downloaded HERE
(NB: References for Figure 1 can be found HERE)
References
1. Deutz NE, et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin Nutr. 2014; 33: 929-36.
2. Cruz-Jentoft A, Sayer A. Sarcopenia. The Lancet. 2019; 393(10191): 2636-2646.
3. Kenny RA, Romero-Ortuno R, Kumar P. Falls in older adults. Medicine. 2017; 45(1):28-33.
4. Bozzetti F. Forcing the vicious circle: sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann Oncol. 2017; 28(9):2107-2118.
5. Byun MK, et al. Sarcopenia correlates with systemic inflammation in COPD. Int Journal Chron Obstruct Pulmon Dis. 2017: 12;669—67.
6. Springer J, Springer JI, Anker SD. Muscle wasting and sarcopenia in heart failure and beyond: update 2017. ESC Heart Fail. 2017; 4(4):492-498.
7. Landi, F et al. The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int. 2017; 28(5):1569-1576.
-
Nutritional Status of Covid and Long Covid Patients
Should we be Paying More Attention to the Nutritional Status of Covid and Long Covid Patients?
 In December 2020 NICE published a COVID-19 rapid guideline on managing the long-term effects of COVID-19. However despite the fact that the current pandemic has highlighted the importance of nutritional status in maintaining good health, nutrition support does not feature in this guidance.
In December 2020 NICE published a COVID-19 rapid guideline on managing the long-term effects of COVID-19. However despite the fact that the current pandemic has highlighted the importance of nutritional status in maintaining good health, nutrition support does not feature in this guidance.Many of the signs and symptoms noted to frequently persist after acute COVID infection, such as breathlessness, fatigue, loss of smell and taste and inflammation, can impact oral intake and potentially worsen nutritional status1-5.
The nutritional consequences of COVID-19 are not yet fully understood but knowledge from acute respiratory distress syndrome suggests that patients are likely to experience skeletal muscle dysfunction which can persist for weeks to years6. Initial recent research has found a very high incidence of weight loss and risk of malnutrition among COVID-19 survivors, independent of hospitalisation7 and sarcopenia, loss of muscle mass and function, has been found to occur in survivors of COVID-19; with older adults and the most critically unwell patients being the most at risk8.
-
Nutritional Status of Covid and Long Covid Patients: READ MORE
Low muscle mass negatively affects patient outcomes and increases healthcare utilisation. It is associated with higher rates of infections, poorer tolerance to chemotherapy, hospitalisation, fractures, reduced quality of life, and reduced survival9. For those with pre-existing conditions (including poor cardiometabolic health), who have had severe COVID-19 and in some cases long COVID, a tailored nutritional approach is likely to be required.
"Whilst more research needs to be done into recovery from COVID and Long COVID, from what we know in relation to other long term illnesses, diet and resistance training are likely to play an important role in assisting in recovery" says Anne Holdoway, Consultant Dietitian, Chair of the Malnutrition Pathway panel and Chair of the British Dietetic Association COVID-19 Clinical Guidance Group. "Amongst those with pre-existing conditions, determining the optimum diet can be complex. Registered dietitians possess the skills to assess nutritional status, oral intake, social status and concurrent medical conditions and can provide an individual with meaningful and appropriate advice to not only optimise recovery but manage underlying conditions and weight, to optimise long-term health through dietary change."
Obesity May Mask Malnutrition
Obesity is common in COVID-19 patients and has been shown to increase the risk for hospitalisation and poorer outcomes10 however obesity may mask malnutrition and muscle loss in COVID-19 patients.
Individuals who are obese, or have comorbidities including type 2 diabetes and heart disease, may experience significant weight loss during acute infection, of which a large proportion may be muscle mass7. This is supported by evidence that a large proportion of patients describe ongoing muscle weakness following COVID-19 infection, as well as an increase in care dependency and frailty scores11,12. While appetite may return to normal after acute infection, inadequate protein intakes and reduced mobility (due to persistent fatigue or breathlessness for example) can result in loss of muscle mass and strength (sarcopenia) even in those who are overweight or obese. For these patients, once acute infection has passed and appetite is normal, a high calorie diet may not be appropriate, and may exacerbate pre-existing conditions, however advice on adequate protein intakes while increasing exercise levels may be needed.
"We know that obesity increases the risk of severe illness and death from COVID-19 and in patients with severe COVID infection who have rapid weight loss, healthcare professionals should be alert to the likelihood of loss in muscle mass (malnutrition) rather than fat mass in some of their patients during the early post hospital period" says Dr Anita Nathan, GP, Malnutrition Pathway panel member. "It is important that messages relating to increased protein intake in combination with exercise are given to these patients to ensure they recover muscle loss."
Nutritional Strategies
Implementing nutritional management strategies is recognised as being crucial for hospitalised patients, particularly those in the ICU or with older age and multi-morbidities13. However recent research suggests that individuals managing or recovering from COVID-19 symptoms at home should receive counselling on how to maintain an adequate intake of calories, protein, and fluids7. It is suggested that strategies such as using remote nutritional screening tools recently developed for primary practise should be implemented to improve the nutritional management of patients managed at home7.
"Where patients may be at risk of malnutrition, for example in vulnerable groups such as people with long term health conditions, or those with Learning Disabilities, we would like to encourage community based healthcare professionals to carry out malnutrition screening following COVID-19 infection" says Liz Anderson, Lead Nurse for Nutrition and Malnutrition Pathway panel member. "This is particularly important where patients are experiencing persisting symptoms that may affect their nutritional status."
INFORMATION ON SCREENING REMOTELY Patients can also be encouraged to SELF SCREEN
For individuals who are underweight or continuing to lose weight following COVID-19 infection, nutrition support in the form of a high energy, high protein diet is indicated, and oral nutritional supplements may be required if patients are unable to increase their intake through diet alone14.
To support community healthcare professionals in the management of patients who have COVID-19 or are recovering from infection the Malnutrition Pathway has developed 'A Community Healthcare Professional Guide to the Nutritional Management of Patients During and After COVID-19 Illness' GO TO GUIDE This includes a COVID-19 specific nutrition care pathway and advice on screening for malnutrition via remote consultations.
The website also features information leaflets designed to help provide appropriate nutritional guidance to patients at low, medium or high risk of malnutrition, along with a resource finder to assist professionals and patients in identifying the correct advice according to the nutritional status of the patient HERE The leaflets include tips on coping with symptoms related to COVID-19 illness and encouraging activity combined with good nutrition. For patients who are not at risk of malnutrition but may have lost muscle mass and strength due to COVID-19 infection and ongoing symptoms, advice should focus on ensuring adequate protein in the diet and increasing physical activity.
"NHS Trusts across the UK are using these resources as part of their discharge packs for COVID-19 patients - in January 2021 alone over 4,000 copies of the COVID-19 and nutrition patients leaflets were downloaded from the malnutrition pathway website" says Anne Holdoway, "With an increasing number of patients now suffering from the longer term effects of COVID-19 we hope that these resources will assist community healthcare professionals in advising patients on the role nutrition can play in aiding their recovery."
A separate guide has been developed for care homes to assist care home staff in the nutritional care of patients who have or are recovering from COVID-19 illness DOWNLOAD GUIDE
Additional fact sheets on incorporating protein into the diet for both healthcare professionals and patients are also available HERE
NB: More detailed support on complex conditions should be sought from a registered dietitian.
Production of the COVID-19 Nutritional materials was made possible by an unrestricted educational grant from Nutricia
References
- Mandal S, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2020.
- Carfí A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. Jama. 2020; 324(6):.603-605.
- Arnold DT, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax 2020.
- Sudre CH, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. medRxiv. 2020
- Doykov, et al. ‘The long tail of Covid-19’-The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Research, 9. 2020
- Files DC, Sanchex MA, Morris PE. A conceptual framework: the early and late phases of skeletal muscle dysfunction in the acute respiratory distress syndrome. Critical care. 2015; 19(1):1-10.
- Di Filippo L, et al. COVID-19 is associated with clinically significant weight loss and risk of malnutrition, independent of hospitalisation: A post-hoc analysis of a prospective cohort study. Clin Nutr. 2020 Oct 29 doi: 10.1016/j.clnu.2020.10.043 [Epub ahead of print]
- Welch C, et al. COVID-19 and Acute Sarcopenia. Aging Dis. 2020 Dec 1;11(6):1345-1351. doi: 10.14336/AD.2020.1014.
- Prado CM, Purcell SA, Alish C, Pereira SL, Deutz NE, Heyland DK, et al. Implications of low muscle mass across the continuum of care: a narrative review. Ann Med. 2018;50(8):675-93.10)
- Huang Y, Lu Y, Huang YM, Wang M, Ling W, Sui Y, et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism: clinical and experimental. 2020;113:154378.
- Vaes AW, et al. Care dependency in non-hospitalized patients with COVID-19. Journal of Clinical Medicine. 2020; 9(9): 2946.
- Huang C, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021.
- Barazzoni R, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39:1631–1638.
- Malnutrition Pathway. A Community Healthcare Professional Guide to the Nutritional Management of Patients During and After COVID-19 Illness. 2020 https://www.malnutritionpathway.co.uk/library/covid19_hcpguide.pdf
-
Malnutrition Awareness Week (5-12 October 2020)
We have a number of free resources available to download on our website to support this years’ Malnutrition Awareness Week including:
Managing Adult Malnutrition in the Community
- MANAGING ADULT MALNUTRITION IN THE COMMUNITY DOCUMENT A practical guide and pathway to assist community healthcare professionals in identifying and managing the 3 million people in the UK at risk of disease-related malnutrition. Developed by a multi-professional team and endorsed by ten key organisations.
- A4 POSTER Managing Malnutrition According To Risk Category Using ‘MUST’ Care Pathway and pathway for using Oral Nutritional Supplements (ONS) in the Management of Malnutrition
Patient leaflets
- Green leaflet: EATING WELL for those at low risk of malnutrition which gives advice on how to eat well and keep as healthy as possible
- Yellow leaflet: MAKING THE MOST OF YOUR FOOD for those at medium risk of malnutrition which provides some simple ideas on how to get the most nutrition from food including food fortification advice
- Red leaflet: NUTRITION DRINKS (known as Oral Nutritional Supplements): for those at high risk of malnutrition which gives advice on incorporating oral nutritional supplements into the diet if they have been prescribed
Fact Sheets
-
FALLS FACT SHEET Outlines key actions for implementing nutrition screening and assessment into falls pathways
- DYSPHAGIA Includes information on the causes, prevalence and clinical consequences of dysphagia plus tips on optimising the diet of individuals with dysphagia including how to identify those who are at risk of malnutrition
- PROTEIN A healthcare professional fact sheet summarises the evidence-based guidelines for protein requirements in ageing and disease, with a useful list of the protein content in everyday foods. This is accompanied by a patient and carer information sheet including advice on getting enough protein from your diet
Care Homes Resources
A number of resources are available to assist those working in care and residential homes these include:
- CARE HOMES FACT SHEET Outlines why older people and the elderly are particularly vulnerable to malnutrition, why is it important for care and residential homes to acknowledge the problem and key considerations for care homes in identifying and managing malnutrition amongst residents
- TOP TEN TIPS FOR CARE HOMES Tips for those working in care homes on the identification and management of malnutrition, including the implementation of care plans and engagement with other care home personnel to create an environment that prevents malnutrition
- CARE PLANS For use with care home residents at low, medium and high risk of malnutrition
- COVID-19 GOOD NUTRITIONAL CARE This guide includes advice for care home staff on dealing with symptoms that may affect the nutritional intake of residents during and after COVID-19 infection
COVID-19 resources
We have recently developed a number of professional and patient materials focusing on nutrition support to assist in recovery from COVID-19 illness:
- A Community Healthcare Professional Guide to the Nutritional Management of Patients, endorsed by BAPEN, BDA and RCN, aims to assist healthcare professionals address nutritional issues of patients with COVID-19 who they may be supporting in the community. It includes a COVID-19 Illness Community Nutrition Support Pathway: GUIDANCE
- This website includes general advice for patients on why nutrition is important to assist in recovery - ADVICE FOR PATIENTS
- Also included is a RESOURCE FINDER to help you to find the correct nutrition advice for you depending on your appetite, weight loss and general overall health. There are 3 leaflets available:
- Green leaflet: EATING WELL AFTER COVID-19 ILLNESS Advice on eating a balanced diet to help maintain strength and fitness and fight infection
- Yellow leaflet: IMPROVING YOUR NUTRITION DURING AND AFTER COVID-19 ILLNESS Advice for those with a poor appetite and/or recent unintentional weight loss, including tips to help get the most from their food.
- Red leaflet: NUTRITION SUPPORT DURING AND AFTER COVID-19 ILLNESS Advice for those who have been very unwell. Aimed at those who have recently been discharged from hospital after COVID-19 illness or who are struggling to eat enough and are underweight and/or have lost quite a bit of weight due to their illness.
For further information on Malnutrition Awareness Week please visit THE BAPEN WEBSITE
-
Information leaflets: good nutrition for COVID-19 recovery
30 April 2020
NEW INFORMATION LEAFLETS TO ADVISE THOSE WITH COVID-19 ILLNESS ON GOOD NUTRITION FOR RECOVERY
While most people infected with COVID-19 will experience mild to moderate illness and recover without requiring special treatment, some may develop more serious illness. Older people and those with underlying medical problems like high blood pressure, heart disease, diabetes, chronic respiratory disease and cancer are more at risk of developing serious disease.
There are no specific foods or vitamin or mineral supplements that will prevent you from catching COVID-19 and good hygiene practice remains the best means of avoiding infection. However, eating a well-balanced diet can help support the normal functioning of the immune system to help fight off infection.
The Managing Adult Malnutrition in the Community team has worked with the British Dietetic Association (BDA) and the British Association for Parenteral and Enteral Nutrition (BAPEN) to develop a range of patient information leaflets to advise those who have COVID-19 illness, or who are recovering after the illness, on eating well to assist in their recovery.
“Dietary advice for people who have or have had COVID-19 illness needs to be considered in relation to a number of factors including severity of their illness, any underlying conditions they have, whether their appetite has been affected and if they are overweight or underweight“ says Anne Holdoway, Consultant Dietitian. “One size does not fit all when it comes to diet and for this reason we have developed a number of different resources to enable people to access the dietary advice most suited to their need. For those who needed support on intensive care I would emphasise the need for individualised dietary advice by a registered dietitian.”
Three different nutritional information leaflets have been developed, each tailored to the differing nutritional requirements of individuals who have been affected by COVID-19. The leaflets aim to help those who have had a mild/moderate illness and have been coping at home and also for those who have been in hospital with a more serious illness. THE LEAFLETS ARE FREE TO DOWNLOAD.
A USEFUL TOOL has been developed on the website to enable people who have or have had COVID-19 to identify the nutritional advice leaflet that is most suitable to their needs
“Fighting off infection can increase your body’s needs for energy, protein, vitamins and minerals, but being unwell can make it difficult to eat and drink enough”, says Liz Anderson, Nutrition Nurse Specialist, “because of this, you may need to think differently about you are eating and drinking. Those who have had a serious case of COVID-19 and particularly those leaving hospital may require additional dietary support in order to regain lost muscle mass. These leaflets offer practical nutritional advice for people who have been affected by the illness.”
Nutritional information for people during and after COVID-19 illness
The three leaflets include tips on for coping with symptoms related to COVID-19 illness and encouraging activity combined with good nutrition:
GREEN LEAFLET - ‘Eating Well During and After COVID-19 Illness’
An information leaflet about eating a balanced diet to help maintain your strength and fitness, as well as help your body fight infection
YELLOW LEAFLET - ‘Improving your Nutrition During and After COVID-19 Illness’
An information leaflet for those with a poor appetite and/or recent unintentional weight loss, including tips to help get the most from their food.
RED LEAFLET - ‘Nutrition Support During and After COVID-19 Illness’
An information leaflet for those who have been very unwell. Aimed at those who have recently been discharged from hospital after COVID-19 illness or who are struggling to eat enough and are underweight and/or have lost quite a bit of weight due to their illness. This information leaflet gives advice on increasing nutritional intake and how to incorporate oral nutritional supplements into the diet if they are prescribed.
Information for those who have not had COVID-19 but are concerned about their nutritional health
For individuals who have not had COVID-19 but are concerned about your overall nutritional health there are a number of LEAFLETS AVAILABLE to help you with healthy eating on the malnutrition pathway website
The British Dietetic Association also offers advice on HEALTHY EATING DURING SOCIAL ISOLATION
Anyone who is concerned about any aspect of their diet or any symptoms of their illness should speak to a healthcare professional for further advice.
NB: Production of the COVID-19 Nutritional materials was made possible by an unrestricted educational grant from Nutricia Advanced Medical Nutrition.
- Anne Holdoway, Consultant Dietitian is:
- • Chair of the Managing Adult Malnutrition in the Community and Managing Malnutrition in COPD panels
- • Chair of the British Dietetic Association (BDA) COVID-19 Clinical Guidance Group
- • Education Officer for the British Association of Parenteral and Enteral Nutrition (BAPEN)
- Liz Anderson, Nutrition Nurse Specialist is:
- • Nurse member of the Managing Adult Malnutrition in the Community and Managing Malnutrition in COPD panels
- • Executive Officer at the British Association of Parenteral and Enteral Nutrition (BAPEN)
-
Updated guidance: combat malnutrition in patients with COPD
Updated guidance to help combat malnutrition in patients with COPD
With research showing that around 1 in 3 inpatients1 and 1 in 5 outpatients2 with Chronic Obstructive Pulmonary Disease (COPD) are at risk of malnutrition, the ‘Managing Malnutrition in COPD’ multi-professional panel has updated its guidance for healthcare professionals and supporting patient information leaflets. It is hoped that the document based on clinical evidence, clinical experience and best practice will raise awareness amongst the multi-disciplinary team of incorporating nutrition screening and nutritional care into management pathways for patients with COPD.
The causes of malnutrition in patients with COPD are varied and include not only the physiological effects of the disease such as breathlessness and fatigue interfering with appetite and the ability to eat but also psychological, social and environmental factors such as depression, social isolation and living conditions. In addition, individuals with COPD may have increased energy requirements arising from systemic inflammation and increased effort associated with breathing. Malnutrition can develop over several years or be precipitated and continue following an acute exacerbation. Sarcopenia (loss of skeletal muscle mass and strength) affects 15% of patients with stable COPD and impairs function and health status3. In addition, nearly a quarter of all individuals with COPD will develop cachexia (loss of lean tissue mass due to chronic illness)4.
The consequences of malnutrition in COPD are significant and contribute to increased healthcare useage and costs, higher mortality, longer hospital stays, more frequent readmissions as well as reduced muscle strength and respiratory muscle function5-14.
‘Managing Malnutrition in COPD’
‘Managing Malnutrition in COPD’ is a practical guide that aims to assist healthcare professionals in identifying and managing people with COPD who are at risk of disease-related malnutrition and includes a pathway for the appropriate use of Oral Nutritional Supplements (ONS) to support community healthcare professionals. The second edition has been updated to include guidance from NICE NG115 Chronic obstructive pulmonary disease in over 16s: diagnosis and management)15 and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy16 as well as including revised guidance on energy and protein requirements for patients with COPD17-19 and advice on nutritional intervention alongside pulmonary rehabilitation programmes which have been found to be associated with improved patient outcomes15, 20-23.
The first edition of the guidance was launched in 2016 and it complements the ‘Managing Adult Malnutrition in the Community’ guidelines (www.malnutritionpathway.co.uk)24 which were launched in 2012.
Patient leaflets
The guidance is accompanied by three complementary colour-coded patient leaflets all of which contain dietary advice, advice on eating and physical activity. They also contain tips on coping with common symptoms of COPD including dry mouth, taste changes and shortness of breath. In addition the red (high risk) leaflet includes advice for patients on incorporating oral nutritional supplements into their diet. The three leaflets are:
- GREEN LEAFLET – ‘Eating Well for Your Lungs’ – for patients at low risk of malnutrition
- YELLOW LEAFLET – ‘Improving Your Nutrition in COPD’ – for patients at medium risk of malnutrition
- RED LEAFLET – ‘Nutrition Support in COPD’ – for patients at high risk of malnutrition
- The Association of Chartered Physiotherapists in Respiratory Care (ACPRC)
- The Association of Respiratory Nurse Specialists (ARNS)
- The British Association For Parenteral And Enteral Nutrition (BAPEN)
- The British Dietetic Association (BDA)
- The British Lung Foundation (BLF)
- Education for Health
- The National Nurses Nutrition Group (NNNG)
- The Primary Care Respiratory Society (PCRS)
- The Royal College Of General Practitioners (RCGP)
- The Royal College Of Nursing (RCN)
‘Managing Malnutrition in COPD’ and the complimentary patient leaflets have been developed by a multi-professional panel, with expertise and an interest in malnutrition and COPD, and is endorsed by ten key professional and patient organisations including the British Dietetic Association (BDA), The British Association For Parenteral And Enteral Nutrition (BAPEN), the Association of Respiratory Nurse Specialists (ARNS), the British Lung Foundation (BLF), the Royal College of Nursing (RCN) and the Royal College of General Practitioners (RCGP)25. The document is based on clinical experience and evidence alongside accepted best practice. All materials can be downloaded for free HERE
What the experts say about ‘Managing Malnutrition in COPD’
“Patients with COPD are particularly susceptible to loss of muscle mass so dietary advice is paramount and in many cases nutritional interventions may be necessary to ensure loss of weight and muscle mass are minimised particularly when patients are undergoing acute exacerbations,” says panel member Dr Peter Collins, Registered Dietitian and Senior Lecturer in Nutrition & Dietetics. “By working closely with the multi-professional team we can make sure that patients at risk of malnutrition are identified and that an appropriate nutritional care plan is put in place whilst ensuring and that those who require a more detailed dietetic assessment are referred on to the Dietitian. I hope that these guidelines will raise awareness of the importance of nutritional intervention in patients with COPD and assist healthcare professionals in incorporating nutrition screening and management advice into the care pathway of patients with COPD.”
“I think GPs are becoming aware of the role that good nutrition plays in achieving better disease outcomes but it is not routinely seen as a priority to incorporate nutrition into treatment plans” says panel member Dr Anita Nathan, General Practitioner/Member of the GPs Interested in Nutrition Group. “With growing numbers of elderly patients and those with multi-morbidities we are going to see a larger group of malnourished patients in our surgeries. We therefore need to work more closely with our dietetic colleagues to ensure nutrition screening and monitoring is integrated into current pathways of care, particularly targeting high risk groups, such as patients with COPD. I hope that these guidelines will assist GPs and other members of the primary care team to facilitate better care for our patients.”
“ARNS has been delighted to be involved with the development and update of these guidelines” says Joanne King, Consultant Respiratory Nurse and panel representative for the Association of Respiratory Nurse Specialists (ARNS). “The first edition of the guidelines and the complimentary patient leaflets have been taken up widely by respiratory nurses across the UK and I hope they will find the updates in the guidance of assistance. By engaging with the multi-professional team in identifying and treating malnutrition we can offer continuity of nutritional care for patients leading to better outcomes and quality of life for patients.”
“Pulmonary rehabilitation plays a key role in the management of individuals with COPD and research suggests that if we can incorporate nutrition intervention alongside exercise programmes we get improved patient outcomes” says Sally King, Respiratory Specialist Physiotherapist and member of the ‘Managing Malnutrition in COPD’ panel. “It is important that we work closely with our dietetic colleagues and the multi-professional team to identify and treat malnutrition to ensure a better quality of life for patients. I hope this guidance will assist physiotherapists in giving appropriate dietary information to support the effectiveness of exercise programmes in patients who are malnourished.”
NB: Production of the ‘Managing Malnutrition in COPD’ materials was made possible by an unrestricted educational grant from Nutricia Advanced Medical Nutrition
References
1. Steer J et al. P117 Comparison of indices of nutritional status in prediction of in-hospital mortality and early readmission of patients with acute exacerbations of COPD. Thorax. 2010; 65(4): A127-A.
2. Collins PF et al. Prevalence of malnutrition in outpatients with chronic obstructive pulmonary disease. Proc Nut Soc. 2010; 69(Issue OCE2): E148
3. Jones et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 2015;70 (3).
4. Wagner PD. Possible mechanisms underlying the development of cachexia in COPD. ERJ 2008; 31: 492-501
5. Collins PF et al. An economic analysis of the costs associated with weight status in chronic obstructive pulmonary disease (COPD). Proc Nut Soc. 2011; 70(OCE5): E324
6. Ezzell L and Jensen GL. Malnutrition in chronic obstructive pulmonary disease. Am J Clin Nut. 2000;72(6):1415-16
7. Gupta B et al. Nutritional status of chronic obstructive pulmonary disease patients admitted in hospital with acute exacerbation. J Clin Med Res 2010 Mar 20;2(2):68-74
8. Collins PF et al. ‘MUST’ predicts 1-year survival in outpatients with chronic obstructive pulmonary disease. Clin Nutr. 2010;5(2): 17.
9. Collins PF et al. The impact of malnutrition on hospitalisation and mortality in outpatients with chronic obstructive pulmonary disease. Proc Nutr Soc 2010; 69(OCE2)
10. Landbo C et al. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999; 160(6):1856-1861.
11. Vestbo J et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med 2006; 173(1):79-83.
12. Vermeeren MA et al. Prevalence of nutritional depletion in a large outpatient population of patients with COPD. Respir Med, 2006 Aug;100(8):1349-55
13. Ingadottir AR et al. Two components of the new ESPEN diagnostic criteria for malnutrition are independent predictors of lung function in hospitalized patients with chronic obstructive pulmonary disease (COPD). Clinical Nutr 2018; 37(4): 1323-1331
14. Ingadottir AR et al. Association of energy and protein intakes with length of stay, readmission and mortality in hospitalised patients with chronic obstructive pulmonary disease. Br J Nutr 2018; 119(05): 543-551
15. National Institute for Health and Clinical Excellence (NICE) Chronic obstructive pulmonary disease in over 16s: diagnosis and management. NICE Guideline NG115. Dec 2018 https://www.nice.org.uk/guidance/ng115/chapter/Context
16. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. 2019. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf
17. Gandy J. Manual of Dietetic Practice. 6th Ed. Blackwell Publishing; 2019.
18. Parenteral and Enteral Nutrition Group (PENG). Pocket Guide to Clinical Nutrition. British Dietetic Association (BDA). 2019.
19. Bauer J et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE study group.J Am Med Dir Assoc. 2013; 14(8): 542–559.
20. Collins PF et al. Nutritional support and functional capacity in chronic obstructive pulmonary disease: a systematic review and meta-analysis.Respirology 2013; 18:616-629.
21. Sugawara K et al. Effects of nutritional supplementation combined with low intensity exercise in malnourished patients with COPD. Resp Med. 2010 Dec;104(12):1883-9
22. Van Wetering CR et al. Efficacy and costs of nutritional rehabilitation in muscle-wasted patients with chronic obstructive pulmonary disease in a community-based setting: a pre-specified subgroup analysis of the INTERCOM trial. J Am Med Dir Assoc. 2010 Mar;11(3):179-87
23. Schols AM et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J 2014; 44:1504-1520
24. Managing Adult Malnutrition in the Community. Holdoway A. (panel chair). 2012. United Kingdom. www.malnutritionpathway.co.uk
25. The ‘Managing Malnutrition in COPD’ document and supporting patient materials have been supported by 10 key professional and patient associations:
In addition the guidance also includes the following NICE endorsement statement:
‘This guide (www.malnutritionpathway.co.uk/copd) accurately reflects some of the recommendations on malnutrition in the NICE guidelines on nutrition support in adults (www.nice.org.uk/Guidance/CG32) and chronic obstructive pulmonary disease in over 16s (www.nice.org.uk/guidance/ng115). It also supports statements 1,3 and 5 in the NICE quality standard for nutrition support in adults (www.nice.org.uk/guidance/qs24). This resource is intended for use with adults and not children.
National Institute for Health and Care Excellence. Renewed, December 2019
Further Information
We can be contacted regarding the malnutrition pathway materials and website